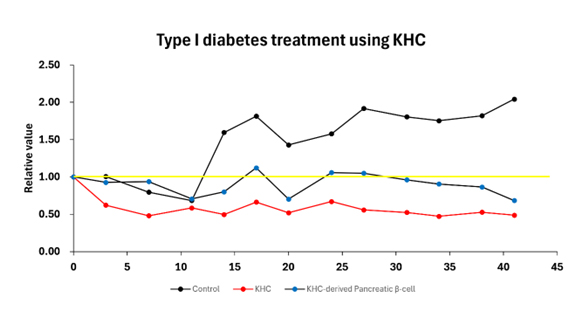
Diabetes is a metabolic disease characterized by chronic hyperglycemia due to malfunctioning of the body's blood sugar regulation system.
It is classified into type 1 and type 2 diabetes.
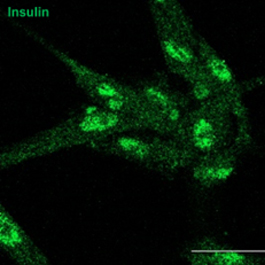
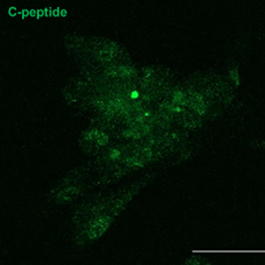
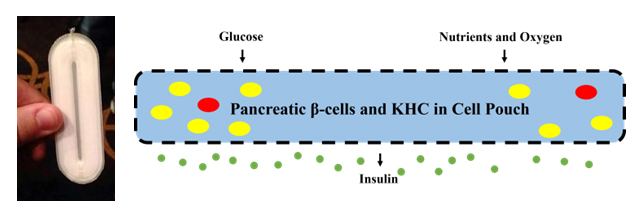
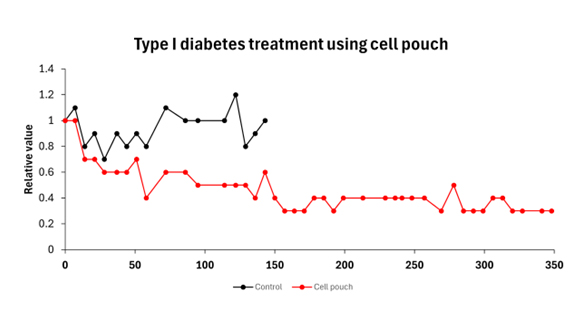
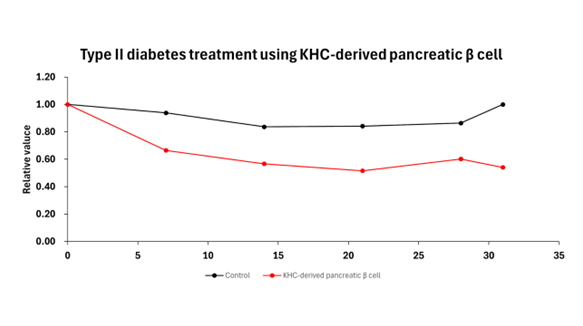
The goal of stem cell therapy for diabetes is to restore the ability to regulate blood sugar by repairing or replacing damaged pancreatic beta cells and modulating autoimmune responses.